NOBSCOTDENTAL CARE
REZA M. MADANI, DMD, FAGD
Common Questions
Our office provides smile makeovers to achieve the beautiful, natural look you seek. We can reshape your natural teeth to make them straighter or more youthful in appeal. Our offices is easily accessible and makes it convenient to those living in Framingham to get the care they deserve.
Make an Appointment
Call Us Today
(508) 877-0800

Before any oral surgical procedure you should:
- Eat a light and easily digestible meal the night before your appointment
- If you are going to be sedated, DO NOT eat or drink anything on the day of your appointment
- Wear short sleeves and loose-fitting clothing
- Arrange for a relative or friend to stay in the office with you and be ready to drive you home
- You may NOT drive a car on the day of the surgery if you are to be sedated!

Fold a piece of clean gauze into a pad thick enough to bite on and place directly on the extraction site. Apply moderate pressure by closing the teeth firmly over the pad. Maintain this pressure for about 30 minutes. If the pad becomes soaked, replace it with a clean one as necessary. Do not suck on the extraction site (as with a straw). A slight amount of blood may leak at the extraction site until a clot forms. However, if heavy bleeding continues, call your dentist. (Remember, though, that a lot of saliva and a little blood can look like a lot of bleeding.)
The Blood Clot
After an extraction, a blood clot forms in the tooth socket. This clot is an important part of the normal healing process. You should therefore avoid activities that might disturb the clot.
Here's how to protect it:
- Do not smoke, rinse your mouth vigorously or drink through a straw for 24 hours.
- Do not clean the teeth next to the healing tooth socket for the rest of the day. You should, however, brush and floss your other teeth thoroughly. Gently rinse your mouth afterwards.
- Limit strenuous activity for 24 hours after the extraction. This will reduce bleeding and help the blood clot to form. Get plenty of rest.
- If you have sutures, your dentist will instruct you when to return to have them removed.
Medication
Your dentist may prescribe medication to control pain and prevent infection. Use it only as directed. If the medication prescribed does not seem to work for you, do not increase the dosage. Please call your dentist immediately if you have prolonged or severe pain, swelling, bleeding, or fever.
Swelling & Pain
After a tooth is removed, you may have some discomfort and notice some swelling. You can help reduce swelling and pain by applying cold compresses to the face. An ice bag or cold, moist cloth can be used periodically. Ice should be used only for the first day. Apply heat tomorrow if needed. Be sure to follow your doctor's instructions.
Diet
After the extraction, drink lots of liquids and eat soft, nutritious foods. Avoid alcoholic beverages and hot liquids. Begin eating solid foods the next day or as soon as you can chew comfortably. For about two days, try to chew food on the side opposite the extraction site. If you are troubled by nausea and vomiting, call your dentist for advice.
Rinsing
The day after the extraction, gently rinse your mouth with warm salt water (teaspoon of salt in an 8 oz. glass of warm water). Rinsing after meals is important to keep food particles away from the extraction site. Do not rinse vigorously!
Anesthesia - The feeling of numbness will begin to wear off in 30 minutes to 4 hours. Until that time, avoid all hot foods or liquids, and do not chew. This is to prevent accidentally burning or biting the lips, cheeks, inside of your mouth or tongue until the feeling has returned
Gauze Pack - Fold the gauze into a small pack and place over the extraction site and apply firm pressure for one to two hours. Change the gauze pack every 15-30 minutes.
Bleeding - It is normal for the extraction site to bleed slightly or ooze blood for 12 to 24 hours following surgery.
Ice Pack - For the first 2 to 8 hours after surgery, ice packs should be applied to the outside of the face over the area of the extraction site. The ice pack should be held in place for 15 minutes on, and then removed for 15 minutes. Doing this throughout the day will help reduce discomfort and swelling.
Medications - DO NOT TAKE ASPIRIN PRODUCTS due to the possible increase in bleeding potential. If prescription medications were prescribed please follow label instructions carefully. For most extractions, a non-aspirin over the counter pain medication will provide good pain relief. Do not take more than the recommended dosage!
Diet - A liquid or soft diet should be adhered to for the first 12 to 24 hours after surgery. It is important to drink plenty of liquids for the first day or two. Avoid the use of a straw as it may dislodge the blood clot that is forming in the extraction site.
Oral Hygiene - Clean the rest of your mouth as usual, however avoid bumping or brushing the extraction site. DO NOT RINSE OR SWISH YOUR MOUTH for the first 24 hours following surgery.
Possible Complications:
Dry Socket - This is sometimes a problem after surgery. The symptoms associated with dry socket are constant moderate to severe pain, bad taste, putrid odor, and poor clot formation at the surgical site. If you think you have ANY of these symptoms call our office as soon as possible.
Fever - Monitor your temperature for the first 24 to 48 hours. Any elevated temperature should be reported to our office.
Swelling - Some swelling during the first 24 to 48 hours can be expected.
1) DO NOT RINSE MOUTH TODAY
Tomorrow rinse mouth gently every 3 to 4 hours (especially after meals) using one quarter teaspoon of salt to a glass of warm water. Continue rinses for several days.
2) BLEEDING
Following extractions, some bleeding is to be expected. If persistent bleeding occurs, place gauze pads over bleeding area and bite down firmly for one-half hour. Repeat if necessary.
3) SWELLING
Ice bag or chopped ice wrapped in a towel should be applied to the operated area; one-half hour on, and one-half hour off for 4-5 hours.
4) PAIN
For mild to average pain, use any non-aspirin type of medication you like. If the doctor prescribes a specific pain medication, follow the instructions and do not mix with other medications unless approved by your doctor.
5) FOOD
Light diet is advisable during the first 24 hours.
6) BONY EDGES
Small sharp bone fragments may work up through the gums during healing. These are not roots; if annoying, return to our office for their simple removal.
7) If any unusual symptoms occur, call the office at once.
8) The proper care following oral surgical procedures will hasten recovery and prevent complications.
Pre-surgical
Q: Is there a food and drink restriction prior to surgery?
A: If treatment calls for the patient to be sedated then yes there are food and/or drink restriction. The patient must not consume anything, including water for 6-8 hours prior to surgery.
Q: Will antibiotics be prescribed prior to surgery?
A: We commonly use antibiotics to kill bacteria found in the mouth, which will also prevent infection after treatment, particularly with the placement of dental implants immediately after extracted teeth. The specific drug used depends on the medical profile and well being of the patient and the type of treatment.
Q: Do I need to avoid certain medications?
A: It is important to discuss all medication with Nobscot Dental Care during your pre-surgical consultation. In most cases medication should be continued unless specifically instructed to withhold them. Typically Plavix, Aspirin, Coumadin and other types of blood thinners can also be continued. When necessary Nobscot Dental Care will consult with your physician to safely manage your medications.
Q: Are the rules different for ORTHOGNATIC SURGERY different from tooth extractions of dental implant placement?
A: Yes, very different. Patients who are undergoing surgical procedures on only one jaw usually go home the same day. Patients who are having surgery on both jaws will generally stay overnight. Generally it is necessary to wire the jaws together after orthognatic surgery. In general, the jaws are immobilized securely with rubber bands for the first 1-2 weeks and then loosely for an additional 3-5 weeks. It is very important to discontinue any medication which are “blood thinners†or which may increase your tendency to bleed. Please stop taking the following medications at least 2 weeks before surgery. Nobscot Dental Care will provide specific instructions prior to your surgery date.
Surgery
Q: Will anesthesia be used?
A: Nobscot Dental Care will discuss your anesthesia options. Our goal is to provide minimal discomfort as possible.
Q: How is the anesthesia administered?
A: Depending upon your treatment we may administer a local anesthesia such as lidocaine or nitrous oxide. For a more involved treatment we may recommend an oral sedation or intravenous sedation.
Q: What do I need to be aware of before intravenous sedation?
A: You may not have anything to eat or drink (including water) for eight (8) hours prior to the appointment. No smoking at least 12 hours before surgery. Ideally, cut down or stop smoking as soon as possible prior to the day of surgery. A responsible adult must accompany the patient to the office, remain in the office during the procedure, and drive the patient home. The patient should not drive a vehicle or operate any machinery for 24 hours following the anesthesia experience. Please wear loose fitting clothing with sleeves which can be rolled up past the elbow, and low-heeled shoes. Contact lenses, jewelry, and dentures must be removed at the time of surgery. Do not wear lipstick, excessive makeup, or nail polish on the day of surgery. If you have an illness such as a cold, sore throat, stomach or bowel upset, please notify the office. If you take routine oral medications, please check with Nobscot Dental Care prior to your surgical date for instructions.
Q: Will my vital signs be monitored during and after treatment?
A: Nobscot Dental Care and/or one of their highly trained surgical assistants will continuously monitor your vital signs.
Q: How long will the surgery take?
A: The length of surgery depends on your treatment. Some surgery's are less than 30 minutes, while other procedures may take considerably longer. Nobscot Dental Care will provide you with the estimated time of surgery at your pre-surgical consultation.
Q: Will there be a lot of bleeding with a tooth extraction?
A: It's important for a blood clot to form to stop the bleeding after a tooth extraction. You will be asked to bite on a gauze pad for 30-45 minutes immediately after the extraction. If the bleeding or oozing still persists, place another gauze pad and bite firmly for another 30 minutes. You may have to do this several times. After the blood clot forms, it is important not to disturb or dislodge the clot as it aids healing. Do not rinse vigorously, suck on straws, smoke, drink alcohol or brush teeth next to the extraction site for 72 hours. These activities will dislodge or dissolve the clot and retard the healing process. Limit vigorous exercise for the next 24 hours as this will increase blood pressure and may cause more bleeding from the extraction site.
Post Surgery
Q: How long is the on-site recovery before I can leave the office?
A: Plan to stay in our recovery room for at least 20 minutes if sedation was involved, or until Nobscot Dental Care is satisfied that you are recovered sufficiently to go home. If your procedure required sedation you must be completely alert before leaving the office for home. You must have a ride home. You may not drive yourself. It is recommend that you do not drive for a minimum 24 hours after surgery.
Q: Will you prescribe antibiotics and pain medication?
A: Procedure and patient health are determining factors of what antibiotic and/or medication will be prescribed. Call the office if the medication does not seem to be working. If antibiotics are prescribed, continue to take them for the indicated length of time, even if signs and symptoms of infection are gone. Drink lots of fluid and eat nutritious soft food on the day of the extraction. You can eat normally as soon as you are comfortable. Dr. Madani will discuss what, when, how long and dosage with you in both the pre-surgery and post surgery interviews.
Recovery
Q: How long will I be off of work/out of school?
A: Depending on the extent of the procedure and type of sedation you may resume work and a normal life style anywhere from a few hours to a few days. It is important to resume your normal dental routine after 24 hours. This should include brushing and flossing your teeth at least once a day. This will speed healing and help keep your mouth fresh and clean. After a few days you will feel fine and can resume your normal activities. If you have heavy bleeding, severe pain, continued swelling for 2-3 days, or a reaction to the medication, call our office immediately.
Q: Will there be swelling or facial bruising?
A: After the tooth is extracted, you may feel some pain and experience some swelling. An ice pack or an unopened bag of frozen peas or corn applied to the area will keep swelling to a minimum. Take pain medications as prescribed. The swelling usually subsides after 48 hours. In some treatments there may be some minor bruising; however, in procedures such as dental implant placement ordinarily there is no bruising seen. For teeth removal or jaw procedures, women and/or very light skinned patients may experience slight bruising. Taking blood thinner will help reduce bruising. It is, however, not uncommon to have a black eye or discolored cheek or neck following extensive procedures. Nobscot Dental Care will discuss what bruising if any would be related to your procedure treatment.

What you eat affects the air you exhale. Certain foods, such as garlic and onions, contribute to objectionable breath odor. Once the food is absorbed into the bloodstream, it is transferred to the lungs, where it is expelled. The odors will continue until the body eliminates the food. People who diet may develop unpleasant breath from infrequent eating. If you don't brush and floss daily, particles of food remain in the mouth, collecting bacteria, which can cause bad breath. Food that collects between the teeth, on the tongue and around the gums can rot, leaving an unpleasant odor. Dry mouth occurs when the flow of saliva decreases. Saliva is necessary to cleanse the mouth and remove particles that may cause odor. Dry mouth may be caused by various medications, salivary gland problems or continuously breathing through the mouth. Tobacco products cause bad breath, so if you use tobacco, ask your dentist for tips on kicking the habit. Bad breath may also be the sign of a medical disorder, such as a local infection in the respiratory tract, chronic sinusitis, postnasal drip, chronic bronchitis, diabetes, gastrointestinal disturbance, liver or kidney ailment.
Bruxism, commonly known as "tooth grinding," is the process of clenching together and the grinding of the upper and lower teeth. During sleep, the biting force of clenched jaws can be up to six times greater than during waking hours.
Bruxism can cause complications over the years:
- Wear down tooth enamel
- Break fillings or other dental work
- Worsening of TMJ dysfunction
- Create jaw pain,toothaches, headaches, or earaches
- Cause tooth sensitivity
- Increase tooth mobility
- Chip Teeth
There is no cure for bruxism; however, the condition can be managed. The most common procedure to help to alleviate pain and discomfort is a Nightguard.

Canker sores are common in adults and children and generally tend to cause discomfort, particularly during eating. Although several factors have been named as possible "causes" of aphthous ulcers, trauma is the most common trigger for them. It has also been observed that they appear in patients who are under stress, or those experiencing health problems. They have also been attributed to hormonal changes, and to some types of dietary deficiencies (i.e., Vitamin B12, Iron, Folic Acid, etc.). Although there is no specific treatment for the ulcer itself, except for severe cases (where usually steroids are prescribed); treatment is usually focused on the pain caused by the ulceration.

Recurrent Herpes Labialis (the common dental term) is a very common viral infection in children and adults. It is caused in most cases by a sub-type of the Herpes Virus, and in most patients it is preceded by an illness (a cold), exposure to sun or exposure to cold. Most patients experience what is known as 'prodromic' symptoms such as itching or burning sensation in the area where the blisters soon appear. This information may allow your dentist to recommend therapies that may minimize or eliminate the appearance of the blisters. This infection is usually self limiting and can last up to 14 days before the scabs fall off.

Saliva flow is important other than appearance and comfort. It keeps the mouth moist and aids in chewing, swallowing, digestion and speech. Dry mouth is a condition from the lack normal saliva flow.
Causes of dry mouth:
- Dehydration
- Emotional Stress
- Anemia
- Related to surgery
- Medical Conditions
- Medication
- Allergy
- Anti-depressant
- Blood pressure
- Some mouth washes high in alcohol content
Dry mouth symptoms:
- Mouth feels sticky
- Lips cracked and dry
- Tongue may have burning sensation
People who experience dry mouth are at high risk for developing:
- Cavities
- Gum disease
- Bad breath
Helping dry mouth:
- Chewing gum / lozenges
- Humidifier at night
- Maintaining good oral hygiene

Accidents can happen during any physical activity. A mouth protector can help protect the soft tissues of your tongue, lips and cheek lining. Over-the-counter stock mouth protectors are inexpensive, pre-formed and ready-to-wear. Boil and bite mouth protectors offer a better fit than stock mouth protectors. Softened in water, they are more adaptable to the shape of your mouth. Custom-fitted mouth protectors are made by your dentist for you personally. They are more expensive, but a properly fitted mouth protector will stay in place while you are wearing it, making it easy for you to talk and breathe.

Oral piercings can be bad for your health. Because your mouth contains millions of bacteria, infection is a common complication of oral piercing. Pain and swelling are other side effects of piercing. Your tongue (a popular piercing site in the mouth) could swell large enough to close off your airway. Piercings can also cause uncontrollable bleeding or nerve damage. The jewelry itself also presents some hazards. You can choke on any studs, barbells or hoops that come loose in your mouth, and contact with the jewelry can chip or crack your teeth.

We ask that our female patients who are pregnant or think they possibly could be to inform us prior to your x-ray examination and dental treatment.
You are probably familiar with the links between tobacco use and lung disease, cancer and cardiovascular disease.
Current studies have also established that tobacco smoking not only causes direct damage to your mouth but also makes periodontal diseases more damaging and harder to treat.
There is a greater incidence of calculus formation on teeth, deeper pockets between gums and teeth, more gum recession and more loss of the bone that hold teeth in your mouth. In addition, smokeless tobacco greatly increases your chance of developing oral cancer. Any tobacco usage can complicate the placement of dental implants.
Chemicals in tobacco such as nicotine, which constricts blood vessels, slow down wound healing.
Other chemicals impair the function of your white blood cells which are your first line of defense against infection. The tars contain carcinogens which over time induce cell mutations and cancers.
Quitting tobacco use will lower the risk of your developing cancer and improve the health of your teeth and gums, as well as your heart and lungs.
Smokeless tobacco poses very serious problems including:
- Causes tooth decay
- Eats away your gums
- Leads to tooth loss
- Bad Breath
- Stains your teeth
- Causes oral sensitivity to hot and cold
- Decreases sense of taste and smell
If oral cancer is left untreated long enough, it may even cause death.

There are many types of cracked teeth. The treatment and outcome for your tooth depends on the type, location and severity of the crack.
Unlike a broken bone, a fracture in a cracked tooth will never heal. Early diagnosis is important, even with high magnification and special lighting, it is sometimes difficult to determine the extent of a crack.
A crown will bind and protect the cracked tooth. When a crack reaches the tooth root, root canal treatment is frequently needed to treat the injured pulp. A cracked tooth that is not treated will progressively worsen, eventually resulting in the loss of the tooth.

It is not uncommon for children to inadvertently 'bite' on their lips or cheeks, particularly following a dental visit where local anesthetic was used. The main reason why this occurs is the natural curiosity that a child has about the area of the mouth that is 'numb.' We try our best to explain to children that local anesthesia is temporary and we give them (and their parents) instructions on how to prevent 'lip biting.' In the event that this occurs, please notify our office so we can determine if your son or daughter will require treatment (i.e. antibiotics or pain medicine).
The development of cavities is usually in those hard to see and reach places in your mouth. These are the areas that usually floss can only reach. Cavities are formed when the bacteria in your mouth attaches to food particles and forms plaque. The acid produced by plaque begins to eat away at the tooth if it is left long enough. First the enamel is attacked then the dentin is next, which is where the tooth's nerve fibers are located. Once the decay makes its way to the dentin a filling is need to stop the cavities progress. If it is left untouched it will eventually reach the nerve and a root canal is then needed to repair the tooth.
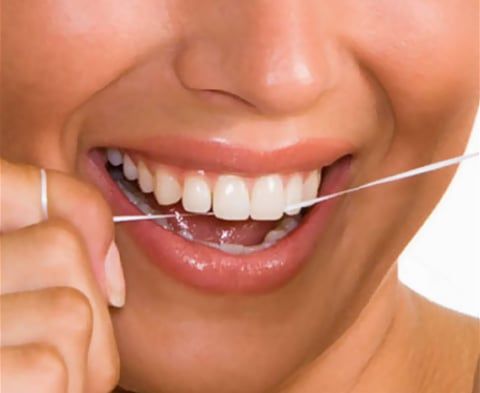
Floss is cheap, so don't be stingy! Tear off about a forearm's length to start. Wrap one end around the middle finger of one hand to "anchor" it and pick up the other end about 4-6 inches away with the middle finger of the other hand. This allows you to manipulate the floss with your thumb and fore finger. As you soil a section of floss, "reel" in another 4-6 inches of clean floss with the anchor finger as you release the floss with the other finger.
Once you get the floss past the tooth contact, move the floss up and down, perpendicular to the tooth. Never shoe-shine the teeth in a back-and-forth motion! You will either notch your teeth or cut your gums, or both!

For most people, a checkup and cleaning every 6 months is standard protocol. Depending on a person's dental health, however, a dental cleaning every 3 to 4 months may be recommended.

For most people, a complete radiographic survey should be done every 3 years, and a "check up" or "recall" set every 6 to 12 months. A complete set of x-rays is estimated to expose you to the same amount of radiation you get on a flight from San Francisco to Seattle.
Doctors use x-rays as an aid in diagnosing problems. Without x-rays, "seeing" the problem will be difficult if not impossible.

In general, the tongue, with its rough surface, is the most common source of bad breath. "Tongue scrapers" are very effective in keeping the tongue clean.

Tooth decay, also know as dental caries, is caused by acids which are produced by bacteria in the presence of sugar. To prevent decay bacteria, sugar and acids must be periodically removed by way of brushing and flossing. Simple tips like, don't sip sugar drinks such as soda, drink the soda straight down as constant sipping is harmful. Ask Dr. Madani for other tips to prevent tooth decay.

Generally speaking, a soft bristled toothbrush is best. Whether you use a manual toothbrush or an electric, anything harder than soft, is too hard. Stiff bristles may give you that clean feeling, but they can also abrade your teeth and cause gum recession.

New patients receive a comprehensive examination which includes a screening for oral cancer, gum and bone disease, blood pressure and systemic disorders. A routine oral exam is performed on established patients to determine any changes in dental and health status since the previous visit. Your gum tissue is measured with a fine instrument ruler to calibrate in millimeters pocket depth between the tooth and the connective gum tissue around the tooth. Pocket depths more than 4 millimeters could indicate disease and infection. The deeper the pocket, the greater the extent plaque bacteria collects and infection in gum disease develops. X-rays are taken as needed. Tooth scaling and root planing occur as needed. Routine cleanings also include a professional polishing (Prophy) that removes only the soft sticky plaque that is above the gum line.
